The Continuity Model of housestaff education
A key component of our internal medicine residency program is our continuity model of housestaff education, which is based on the “four plus one system,” an increasingly popular strategy for compliance with ACGME duty-hour rules. The model’s core is a variation on protected time: each four-week block of inpatient duty is followed by a week dedicated to ambulatory education. This strategy eliminates pressure on trainees to be in two places at once; they no longer rush from inpatient floor to outpatient clinic. Life assumes a consistent rhythm and “sleep debt” is minimized. The system enhances clinical care as well, reducing the fragmentation and waste that sometimes accompany the traditional system, and supporting residents in building a practice over time. Didactics and subspecialty training in both settings benefit from the continuity, and research becomes a real option.
Inpatient medical teams consist of one attending (a teaching hospitalist), one resident (second- or third-year), one or two interns, and several third- and fourth-year medical students. On rounds and at daily chart review sessions, all decision-making and order-writing is done as a team, with a senior resident and supervising attendings. Teams are on a Q4 call cycle. Residents rotate throughout residency to both North Shore University Hospital and Long Island Jewish Medical Center.
Teaching hospitalists round daily with the full team. A night float system handles admissions and cross-coverage from 7pm to 7am. Interns are supervised throughout the day and night, with in-house hospitalist attendings and senior residents on call.
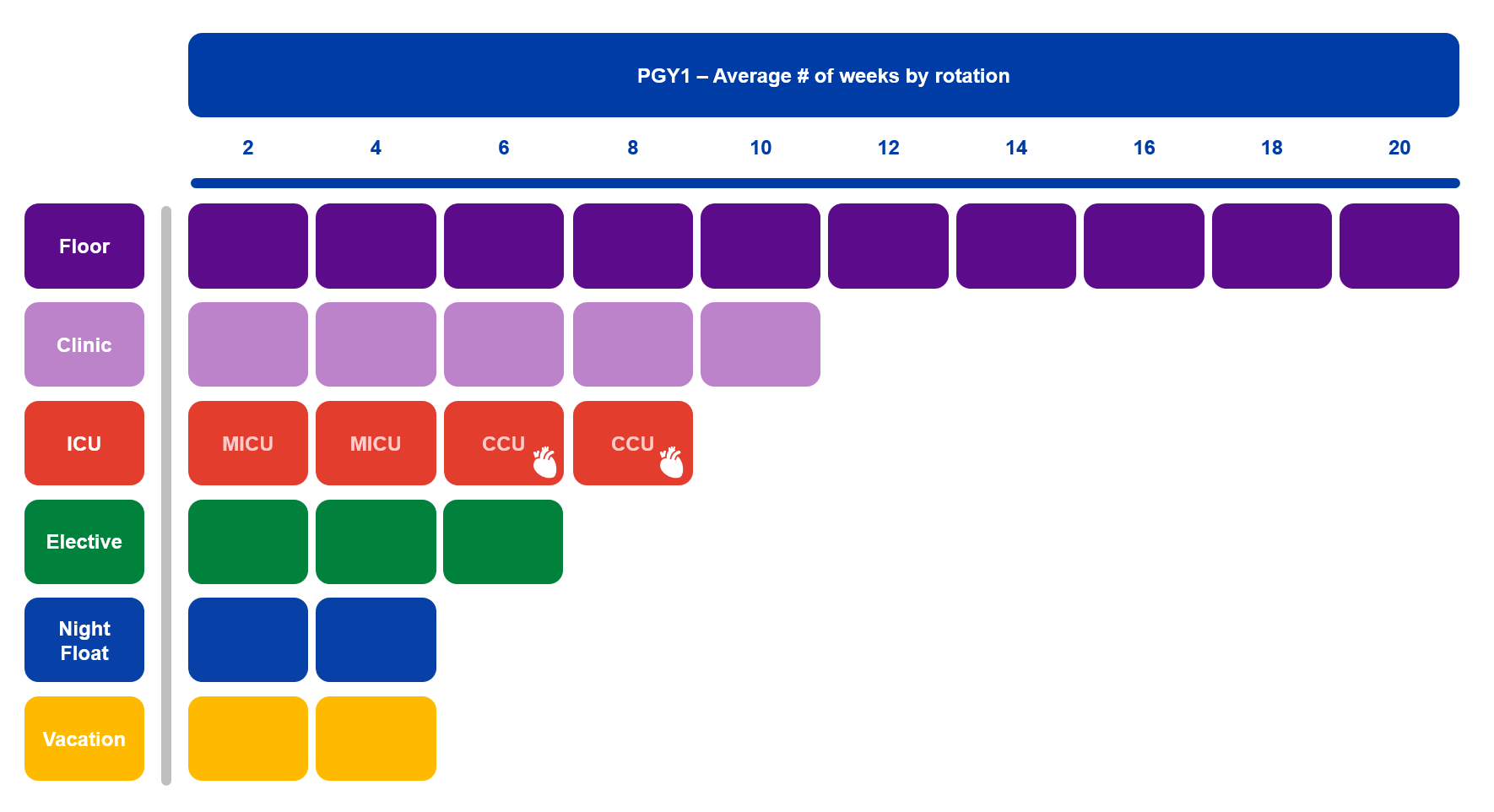
Other inpatient rotations include the medical intensive care units, cardiac care units, ED and subspecialty electives.
The medicine admitting resident (MAR), a third-year resident, screens newly admitted cases in the emergency department to determine which patients will be covered by medicine housestaff, increasing housestaff autonomy.
The ambulatory care programs are responsible for more than 20,000 patient visits annually. Housestaff build a continuity practice over three years and are supervised closely. Each clinic session is precepted by several full-time ambulatory teaching attendings and a chief resident. All cases are presented to a preceptor and discussed in detail. Preceptors observe physical examinations and patient encounters and guide decision-making. Our ambulatory practices at 865 Northern Boulevard and The Medical Subspecialties at Glen Oaks focus on interprofessional primary care with residents working alongside the interprofessional team in teamlets.